Clinical Example: Inclusion Cysts of the Distal Phalanx Excision and Bone Graft
| Intraosseous epidermal inclusion cysts occasionally develop as a late effect of penetrating trauma of the fingertip. They are thought to represent continued growth of cutaneous elements driven into and then trapped into the bone at the time of injury. |
| Click on each image for a larger picture |
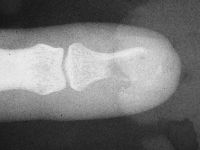
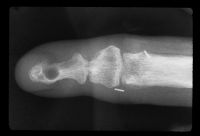
| Case 1. This patient presented with a progressive index finger nail deformity years after an open crush injury of that fingertip. |


| Xrays show loss of much of the distal half of the distal phalanx, with cortical disruption. |

| This was approached through a midlateral incision extended around the tip to allow direct access to the nail bed. |

| A typical whitish smooth epidermal inclusion cyst was found protruding from the tuft of the distal phalanx. |

| The cyst was excised, and the cavity was debrided with a high speed burr. |
| The tuft was reconstructed with an olecranon bone graft. |

| This was sculpted into a tuft shape to provide support for the nail bed. |

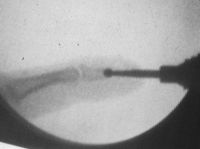
| Graft in place. Exposure facilitated by using 25 gauge needles to convert a Heiss to a Gelpi retractor. |

| Intraoperative films. |



| Result at three months. |


| Donor site. |

| Full range of motion. |



| Case 2. These were the only recognizable digits recovered from the scene after this patient sustained bilateral finger amputations from a rip-cut blade rotating saw injury. |

| Although the middle fingertip is attached, it was devascularized and the palmar soft tissues were destroyed. |

| The amputated ring finger was replanted on the middle finger stump using a modified wraparound technique. |

| The ring distal phalanx was secured to the middle phalanx remnant of the middle finger. |
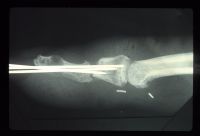
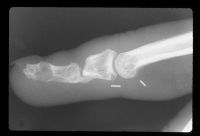
| Late films show only palmar cortical bridging and a lucency in the distal phalanx which was visible in the original films, consistent with an epidermal inclusion cyst. The patient admitted to many open and crushing fingertip injuries over the years in his line of work. |
| A bone graft was used to ablate the tumor and reinforce the bone junction. A midlateral tip incision was used on the side opposite the replantation vascular repair. A midline palmar incision was not used because of concerns regarding devascularizing the tip on the opposite side of the vascular repair. |


| The bone was windowed laterally to remove what was confirmed to be an inclusion cyst. |


| A cortical strut graft and cancellous bone was harvested from the distal radius. |


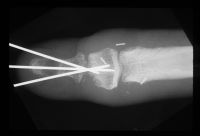
| The graft was sculpted to the diameter of a Steinmann pin. |

| That pin was used as a drill and then replaced with the bone graft. The cyst defect was packed with cancellous bone. |

| Temporary pin placement. |
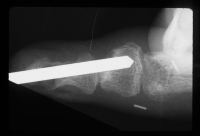


| After tapping the bone graft into place. |



| Late result. |






|
Search for... intraosseous inclusion cyst
|
Case Examples Index Page | e-Hand home |